Andropause, which can begin as early as 30 years old, is described as a stage in a man’s reproductive life characterized by late-onset hypogonadism. It is a stage of steady decline in reproductive function with a prevalence rate linked with advancing age. The main events at andropause are centred around a steady decline in testosterone production and testicular function. Andropause is associated with decreased sexual satisfaction, nervousness, decreased libido, depression, irritability, fatigue, cognitive decline, hot flushes, and sleep disorders. These symptoms adversely affect the quality of life of andropause males. The thyroid hormone and other non-gonadal hormones and responsible for many secondary regulations of the hypothalamic-pituitary-gonadal axis. Sorting the thyroid through consuming thyroid supporting nutraceuticals such as those made available through TriFixx™, can help to better manage the terrible symptoms associated with andropause.
INTRODUCTION
By now, you should have heard a few things about the thyroid gland. As small as it looks, the thyroid gland produces hormones that influence and control metabolic processes and brain functions in the human body. This makes it an important organ worthy of scientific inquiries and studies. Should the thyroid organ be defective, bone development, lipolysis (fat), tissue differentiation (cell change), thermogenesis (warmth), and energy storage will be adversely affected. This explains why the thyroid is considered an important organ in biological sciences. As research inquiries continue to unravel the mysteries surrounding this important organ, various medical reviews have continued to highlight different methods of improving thyroid health.
Men’s Health and Life Expectancy as a Global Issue
Men’s global population ratio is a justification to discuss men’s health. As of 2020, there are approximately 3.93 billion males in the world, representing 50.42% of the total global population. By interpretation, this means the world has 65.15 million more males than females. Currently, the Gender Ratio in the world stands at 101.9 males per 100 females. Talking about men’s health, on many occasions, involves talking about their life stages.
From childhood to adolescence, through andropause to adulthood, men require specialized medical care. In some countries, this medical care is designed as recommended health screenings and vaccinations at different stages of men’s life. Looking at these care plans, you will understand one thing – men, just as women, can also be vulnerable to a whole host of health complications and issues at different stages of their life. These care plans help manage these issues better.
In many climes, men's health is discussed in light of life expectancy and gender differences. According to a 2013 report of the National Center for Health Statistics, the life expectancy for men is pegged at 76 years, about 4 years lesser than the value for women – 81 years. This lower life expectancy has been explained by biological, ethnic, and socio-economic factors. The biological perspective has been explained with many hypotheses such as protection from oxidative stress in women, telomere length, a less active immune system compared with females, the compensatory effect of a second X chromosome, and the protective effect of estrogen in women (Pinkhasov et al., 2010). These differences, many argue, give a natural disadvantage to the male gender and ultimately affect the well-being of men in their lifetime.
Regardless of the cause of death, men generally have a higher mortality rate than women. In 2016, the World Health Organization Statistics revealed that men had a shorter life expectancy than women in all countries (Wang et al.,2010). Depending on the region under review, the risk factors involved are slightly different. Disease trends are well recognized and studied as contributing factors to the lower life expectancy in men. These trends, many times, are affected by income level and other socio-economic determinants. Men from high-income countries appear to have a relatively higher life expectancy than those from low-income countries. In developed countries, non-communicable diseases are the main causes of men's death; in underdeveloped countries, communicable diseases take that position. Male-specific disease conditions are another discourse point in men’s health. This, in addition to health stats records suggesting that men have higher morbidity and mortality from hypertension, diabetes, coronary heart disease, and cancer.
In recent times, hormone-related medical conditions have gained prominence in men’s health. From childhood to adulthood, there are different hormones regulating growth and development in men. Hormonal influence on men’s health is more pronounced at puberty. This stage of transitioning to adolescence witnesses an interplay of hormonal regulations responsible for the development of secondary sex characteristics. Hormone-producing glands play important roles during these life stages. The thyroid hormones and gonadal hormones are responsible for major physiological actions as men age. If these hormone complexes are healthy, men have a better chance at living a quality lifestyle for a lifetime.
Important Thyroid Functions in Men
The thyroid gland is an endocrine gland located in the inferior anterior neck. Primarily, it is responsible for the productions, secretion of thyroid hormones and iodine homeostasis in the body. The main hormones produced by this gland are thyroxine (T4) and triiodothyronine (T3). Calcitonin is another important secretion of the thyroid gland. The effects of the thyroid hormones have been measured and characterized on virtually all nucleated cells in the human body.
Active thyroid hormones increase myocardial contractile force and speed. They are also directly involved in the regulation of basal metabolic rate, heat production, and oxygen consumption rate. Resting respiratory rate and thermogenesis also depends on the physiological health of the thyroid glands.
T3 is responsible for linear bone growth and the development of foetal growth centres. In adulthood, it additionally stimulates bone remodelling and degradation of the mucopolysaccharides and fibronectin in extracellular connective tissues. In the nervous system and gastrointestinal system, thyroid hormones play major roles in stimulatory regulation. These stimulations result in increased wakefulness, alertness, and responsiveness to external stimuli. T3 also interacts with the peripheral nervous system, controlling peripheral reflexes, motility, and gastrointestinal tone (Armstrong et al., 2021).
In recent times, the clinical importance of thyroidal influence on men’s reproductive health has been widely studied. Reproduction events and regulation in males are primarily directed by the hypothalami-hypophyseal testicular axis involving the follicle-stimulating hormone, luteinizing hormone, gonadal steroids, and the hypothalamic gonadotropin-releasing hormone. By exerting modulatory effects on this axis, thyroid hormones have principal control over reproductive functions that characterize male reproduction. Thyroid hormones are readily expressed on the testis, reproductive tract, and accessory sex glands in males. The thyroid hormones bind to these specific nuclear thyroid receptors in these locations to mediate thyroidal effects on male reproduction (Jannini et al., 2000).
Thyroidal functions on male reproduction are complex, prompting much research into the link between thyroid functions and sexual health in ageing men. The studies connecting thyroid hormones with sexual functions in men were first conducted in animal studies. In early studies, rats rendered thyrotoxic by T4 presented with decreased serum gonadotropin level, decrease in total lipids and cholesterol, and decreased phospholipids in testes. Changes to the reproductive secretions and physiology significantly affected the rat’s ability to procreate.
In a 2010 study published by Endocrinology Review, researchers administered larger doses of thyroid hormone to rats and rabbits in a bid to better understand the link between thyroid hormones and reproductive functions of biological systems. Results from this study show that supra-physiological does of T4 results in early maturation and shortens development course in immature male mice less than 4 weeks. Larger doses, however, resulted in decreased testes weights and seminal vesicles in all the animals (Krassas, 2010). By extrapolating the results of these animal studies, scientists have developed human model studies to understand how the thyroid function in the reproductive systems of male humans.
Andropause: A Brief Overview
What have you heard about andropause? Depending on where and how you come about the term, you might have heard people call it different versions – ‘male menopause’, ‘late-onset hypogonadism,' 'male climacteric' or 'androclise’. Saying that andropause is the male version of menopause is not entirely incorrect, the only differences are just in perspectives and hormonal events during this period.
Andropause is described as a stage in a man’s reproductive life characterized by late-onset hypogonadism. It is a stage of steady decline in reproductive function with a prevalence rate linked with advancing age. Although andropause is prominently characterized by a decrease in sexual satisfaction, the events during this stage also affect the general well-being of men as levels of circulating testosterone decreases.
In comparison with menopause in females, andropause is associated with: nervousness, decreased libido, depression, irritability, fatigue, cognitive decline, hot flushes, and sleep disorders. Androgen deficiency during this period of life may adversely affect multiple biological functions, making this stage a terrible experience for many males. A major difference to menopause in females, is that andropause does not occur as a sudden arrest of gonadal function. Gonadal functions only decline steadily, and fertility persists until very old age. As ageing progresses, andropause slowly creeps, and there is a noticeable decline in both endocrine and exocrine testicular functions (Vermeulen, 2000).
Andropause is still a big debate in human medicine as the features that describe this stage remain under investigation. Also, the testosterone level at which andropause occurs is subject to variations in study populations. Except for the age-related decline in sexual drive, many men remain asymptomatic in andropause. In other men, the stage is characterized by general body symptoms that adversely affect the quality of life. The reported prevalence of andropause in men aged 30-69 years is pegged at 3.1 – 7%, while in men older than 70 years, the prevalence rate is pegged at 5.6%. Prevalence generally increases with advancing age (Araujo et al., 2007). On average, only about 5-35% of men receive medical treatment for the symptoms of andropause. This explains why this part of men’s reproductive health has received less attention over the decades.
How Does It Happen?
Just as in menopause with females, andropause is mediated by hormonal regulations that affect reproductive functions. The main events at andropause are centred around a steady decline in testosterone production and testicular function. The decline in testosterone production is primarily testicular in origin. However, the alterations in the hypothalamic-pituitary-gonadal axis, illness, stress, thyroidal dysfunctions, medications, obesity, and psychiatric conditions may have a role in this decline. These conditions are all common in elderly males – the population with the highest prevalence rate of andropause. Currently, the physiological basis of andropause is not as clearly defined as in menopause, but there are many hypotheses under investigation. These include:
- Age-Related Testosterone Decline
The age-related decline in serum testosterone level, causing diminished muscle strength, erectile dysfunctions, and decreased libido, is perhaps the most popular hypothesis today. Beginning in the third decade of life, ageing is associated with serum testosterone decline at a rate of 1% per year (Harman et al., 2001). Circulating testosterone normally binds to serum proteins, especially the sex hormone-binding globulin (SBHG) and albumin. Testosterone bound to SBHG is unavailable for tissue use, but testosterone-bound albumin and free testosterone is. As aging advances, the concentration of SHBG increases significantly, the amount of testosterone bound to this protein increases proportionally. As a result, the concentrations of albumin-bound testosterone and serum-free testosterone decrease gradually. This explains why a larger percentage of older men have lower levels of biologically active testosterone and higher levels of SHBG-bound testosterone, which are unavailable for tissue action.
- The Decline in Hypothalamic Gonadotropin Regulation with Ageing
As stated earlier, reproduction function in males is directed by the hypothalamic-pituitary-gonadal axis. The decline in testosterone production has been linked with inadequate stimulation of luteinizing hormone by this axis. An alteration in normal hormonal regulation of this axis can cause a decline in testis function. Older men, presenting with symptoms that describe andropause, also present with a decreased number of Leydig cells and cells of the testis that produces testosterone. This is similar to the degeneration of oocytes in female menopause and an eventual loss of reproductive ability. As the regulation of the hypothalamic-pituitary-gonadal axis declines, studies have shown that the functions of the seminiferous tubule compartment of the testes also decline. Spermatogenesis is adversely affected, the number of sperms with normal motility and morphology also decreases, but the concentration of ejaculated sperm remains unchanged.
- Other Multifactorial Aetiology of Age-Related Testosterone Decline
Non-gonadal hormone regulations of reproductive functions fall under this hypothesis. This simply means a decline in the secondary contributions of other hormones in the body to male sexual health can also result in andropause. Many studies have documented the decreased serum concentration of DHEA (a weak adrenal androgen that is a precursor to testosterone) as age advances. Alteration in the normal functioning of hormones of the thyroid has also been linked with andropause. Comorbid illnesses including chronic renal failure, liver diseases, and malignancies, and the use of certain medications have also been found to have a controlling influence on andropause. Malnutrition associated with comorbid illnesses is linked with a decreased testosterone level. This hypothesis fits perfectly into the observation that sick old men in nursing homes have a higher prevalence of testosterone deficiency and lower androgen function compared to healthy younger males.
Thyroidal Regulation of Andropause
Hormone replacement therapies have been proposed by many scientists as a treatment option for the undesired symptoms associated with andropause. By understanding how non-gonadal hormones contribute to the regulation of the hypothalamic-pituitary-gonadal axis, scientists can better understand how to manage andropause. The thyroid gland is known to partake in the regulation of male reproductive functions. This is evidenced by the high prevalence of thyroidal dysfunctions in older men presenting with symptoms of andropause. Thyroidal dysfunctions at this stage are an indicator of thyroid hormone deficiency.
Many animal studies have documented evidence suggesting the expression of thyroid hormone receptors in the testes. Thyroid receptors were prominently expressed on the sertoli cells and seminiferous tubules. In an early study published by the Journal of Clinical Endocrinology and Metabolism, the distribution of thyroid hormone nuclear receptors in human testicular tissues was studied and confirmed. By acting on these receptors, T3 regulates the maturation and growth of the testis and controls sertoli and leydig cell proliferation in humans.
Testicular expression of thyroid receptors in sertoli cells explains why hypothyroidism leads to a marked delay in sexual maturation and development (Zamoner et al., 2008). Delayed testicular maturation associated with an inadequate thyroid function has also been linked with reduced serum levels of gonadotropins, follicle-stimulating hormone, and luteinizing hormone. In a recent study, scientists demonstrated how thyroidal function directly affects the regulation of the hypothalamic-pituitary-gonadal axis. Rats submitted to hypothyroidism showed a significant reduction in the pituitary production of luteinizing hormone. The research result also suggests a marked reduction in the amount of serum testosterone concentration (Romano et al., 2013).
The Trials and Tribulations of Andropause
Decreased testosterone functionality in men presents with many symptoms. These symptoms, although not reported in some older men, significantly reduce the quality of life in andropause men. These symptoms often mirror menopausal complaints in women and generally lead to deteriorated general and sexual conditions. The common complaints in andropause men as documented by Wu et al. include:
- Low libido – 91%
- Lack of energy – 89%
- Erectile dysfunction – 79%
- Postprandial somnolence – 77%
- Memory deterioration – 77%
- Loss of pubic hair – 70%
- Sadness and irritability – 68%
- Decreased endurance – 66%
- Loss of facial hair – 55%
- Trouble at work – 51%
Emotional disorders are well described in andropausal men. Moodiness, depression, aggravation, poor concentration, and worse stress management are the commonly diagnosed emotional disturbances in these men. In a 2007 study report, Sato et al. found depressive disorders in approximately 42% of patients in an andrology clinic. Anhedonia – an inability to express joy - is considered the basis of depression in these patients. There is also the persistent feeling of exhaustion, reduced sexual drive, declining cognitive function, and a reduced psychomotor drive.
Managing Andropause Symptoms with an Optimized Thyroid
Hormone replacement therapy is considered a viable option in the management of the symptoms reported by an andropausal man. However, the therapy option has generated much controversy in recent times. Physicians could not agree on a testosterone level below which testosterone replacement therapy should be offered to older men with these symptoms. In its 2010 guidelines, the Endocrine Society recommended against considering testosterone therapy as a general treatment policy for these men. Many studies have since proposed other therapy options.
Andropausal men present with hypothyroidism and other thyroid dysfunctions. This suggests inadequate thyroidal functions and alterations in thyroidal regulation of the hypothalamic-pituitary-gonadal axis. Optimizing thyroid health is considered a more acceptable therapy option. Compared with testosterone therapy, this option is cheap, easily monitored, and not contraindicated in a large population of andropausal men with underlying medical conditions. The recommended methods of optimizing thyroid health include:
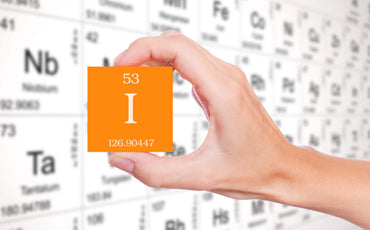
- Adequate Dietary Iodine Intake
Optimizing the thyroid starts with making sure the thyroid gets enough nutrients needed for its primary functions. Iodine is the primary micronutrient required for the production of thyroid hormone. Meeting the recommended intake level in older men - through supplementing with such products as Iodine Fixx™ - can help manage the symptoms associated with andropause.
- Sorting the Thyroid with Nutraceuticals
There are multiple nutraceuticals available to support the thyroid, which can be tailored to the individual, dependent on whether they present as hypothyroid, hyperthyroid, or autoimmune. TriFixx™ provides the public with access to premium grade nutraceuticals, designed specifically for thyroid support. By scoring their symptoms online, consumers are given the power to self-diagnose their symptoms and see which nutraceuticals could best help individuals in their circumstance. TriFixx™ offers men experiencing the terrible symptoms of andropause at the hands of poor thyroid function, an effective solution to their andropausal blues.
Final Thoughts
A decline in testicular functions and level of circulating testosterone is considered the principal physiology of andropause in men. This stage is characterized by a reduced reproductive ability and other symptoms that adversely affect the quality of life of andropausal men. Optimizing the thyroid can better manage the symptoms associated with andropause. The TriFixx™ line of nutraceuticals, help the body produce enough thyroid hormones needed to affect reproductive actions at the sertoli cells and somniferous tubules. A healthy thyroid can help you better manage the symptoms of andropause.
Related Products
REFERENCES
- Armstrong M, Asuka E, Fingeret A. Physiology, Thyroid Function. [Updated 2021 Mar 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-Available from: https://www.ncbi.nlm.nih.gov/books/NBK537039/